Incarcerated people are dying because some facilities within the Illinois Department of Corrections seem to be denying testing or treatment for COVID-19.
While we welcome Illinois’s recent announcement that people who are incarcerated in three facilities will be regularly tested, we’re disturbed it took so many months to make this decision. Restore Justice started asking for widespread testing in prisons as soon as such testing became available to all Illinoisans.
We call on the State to immediately implement this new testing program in every Illinois Department of Corrections (IDOC) facility. While prison employees at each facility will be regularly tested, the State has not announced plans to regularly test incarcerated people at the vast majority of its facilities. COVID-19 has killed 50 incarcerated people since March, with nearly half of those deaths occurring since mid-October, according to the Chicago Tribune. The State does not regularly report COVID-19 deaths and hospitalizations among incarcerated people.
Every day, Restore Justice hears from incarcerated people with COVID-like symptoms who have been denied tests, from people with sick cellmates denied tests despite extremely close proximity, and from people who have tested positive for COVID-19 but are not receiving adequate medical care. The reports point to a disturbing trend: It appears some IDOC employees are actively discouraging both testing and treatment.
We have received consistent, frequent reports from a handful of facilities that staff have threatened to terminate the employment of incarcerated people who ask to be tested because of symptoms or exposure, allowed symptomatic people to remain in the general population, and failed to ensure sick people receive proper treatment.
Restore Justice receives reports because, for more than a decade, our staff and board members have built relationships with a significant number of incarcerated people and their family members. In March 2020, we created a tracker to monitor prison conditions during the pandemic. We have received more than 500 reports in the last nine months. While we have received reports from almost every facility, the most frequent and alarming incidents in November and December have been reported at Hill, Dixon, Illinois River, Lawrence, Pontiac, and Stateville correctional centers.
We do not have access to data that could tell a more complete story, and so we will share three anecdotes that are typical of recent reports in the hope that more dramatic action can be taken to save lives. Most of the people we have spoken with fear retaliation, and so we have only shared names in cases where the incarcerated individual is deceased.
A man died Tuesday, December 1 at Pontiac Correctional Center. Tyrin Smith’s family says staff waited three days to test him after his first symptoms. After testing positive, in an expression of anger, Tyrin threw a bag of ice on the floor, according to the family. Staff put him in the “hole,” leaving him in isolation without hot water, without a mattress, and without the ability to call his loved ones. In an effort to get medical attention, Tyrin went on a hunger strike. But, the staff still ignored his pleas. Tyrin’s family told Restore Justice they called Pontiac and IDOC repeatedly for two weeks, demanding help. They didn’t get any. Tyrin leaves behind a heartbroken fiance, family, and friends both in and out of prison.
It’s important to note, Tyrin died at Pontiac Correctional Center, and incarcerated people at Pontiac are not part of the State’s new testing program. Only those at Dixon, Vandalia, and Logan correctional centers are.
At Dixon Correctional Center, an incarcerated man asked for days to be tested because he was having trouble breathing. The man’s cellmate previously tested positive. Yet, staff would not test the man, even though he felt sick, because he didn’t have a fever. This contradicts the Center for Disease Control’s (CDC) testing recommendations. The CDC encourages testing if you have shortness of breath and/or have been in close contact for more than 15 minutes with someone who has COVID-19. In many prisons, you can touch both sides of a cell at the same time. These cells are smaller than many bathrooms and closets. They certainly fit the criteria of close, sustained contact.
When they finally agreed to test the man incarcerated at Dixon, results confirmed he had COVID-19. Staff did not quarantine him.
At Hill Correctional Center, an incarcerated person requested a test after his co-worker contracted COVID-19. The man told Restore Justice that staff told him, if he took the test, he would lose his job. Jobs are valuable in prison, providing not just financial support but also an outlet and activity. Another incarcerated individual wrote to us about this same case. He said that after the first person tested positive, two people who had been in close contact with the person and who had symptoms remained in the general population for days.
The person who originally tested positive handled food and identification cards for at least 100 other incarcerated people.
These men also told Restore Justice people are not being tested even when their cellmates become seriously ill, matching reports we’ve heard from many facilities.
COVID-19 CASES ARE RISING AT IDOC FACILITIES
COVID-19 cases are spiking at Dixon, Taylorville, Jacksonville, Robinson, and East Moline correctional centers. IDOC has confirmed 468 COVID-19 cases among incarcerated people in Dixon; there are 358 current active cases. The prison’s population is 1,952 people, meaning the positivity rate is currently 24 percent.
Corrections staff confirmed that at Taylorville, there have been 409 confirmed cases and 273 active cases of COVID-19 cases among incarcerated people. With 959 people incarcerated there, the positivity rate is 43 percent.
All other IDOC correctional facilities are close behind Dixon and Taylorville. There are 24 facilities under administrative quarantine, and 21 facilities under full lockdowns. This is extremely concerning because we haven’t yet seen a likely rise in cases after Thanksgiving. We are worried numbers will keep rising.
FLAWS IN IDOC’S COVID-19 RESPONSE
Both recent reports of denial of adequate care and rising case numbers highlight the flaws in IDOC’s COVID-19 response. Early in the pandemic, IDOC failed to make testing and contact tracing a priority; they relied on two other pillars, administrative lockdown and distribution of personal protective equipment (PPE), both of which are important but not an adequate replacement for testing and contact tracing. Regular, widespread testing of incarcerated people and staff could help identify asymptomatic individuals so they are both separated from people without the virus and put in places where they can be well cared for should they become symptomatic. This testing would also provide data to better control the spread of the virus. IDOC must implement such testing at every facility, not just the Dixon, Vandalia, and Logan.
In the early days of the pandemic, Illinois did not report the number of tests administered to incarcerated people. While we applaud IDOC for beginning to report testing numbers as of December 4, the department continues to lag behind peer states in the number of incarcerated people tested and in the frequency of testing. There are 30,888 people incarcerated in IDOC facilities, and the State has reported administering 22,448 tests, as of December 4. This means there are still people incarcerated who have not even once received a COVID-19 test; only 72.6 percent or fewer (if people have had multiple tests) of those incarcerated in IDOC facilities have been tested for COVID-19.
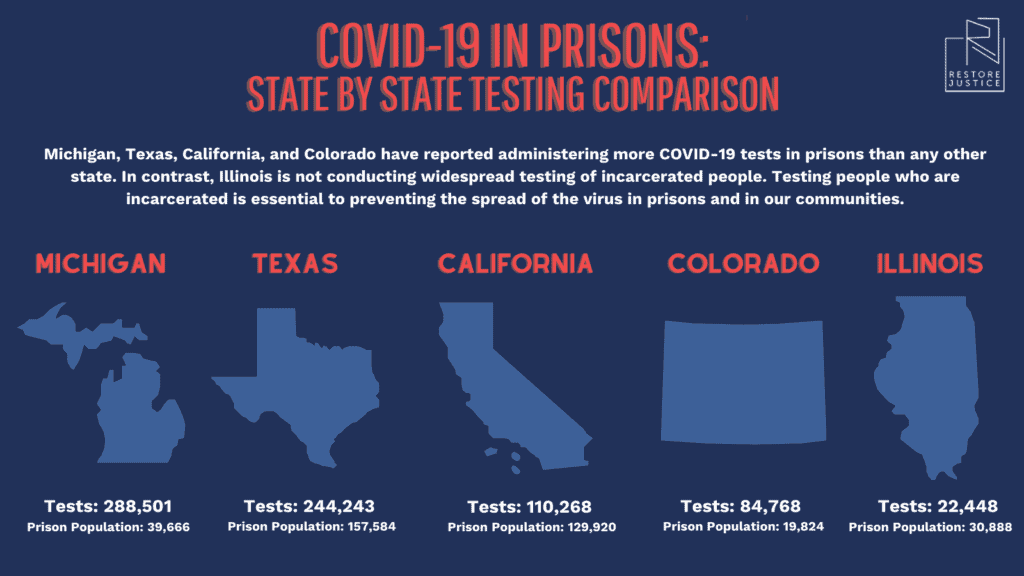
Texas has more incarcerated people than Illinois deos. Despite its large prison population, Texas has still prioritized testing every person in custody. In May, Texas spent $45 million on oral swab testing for prisons with COVID-19 outbreaks.
Illinois’ population is comparable to Michigan’s, yet Illinois is far behind our Midwestern peer in administering COVID-19 tests in prison. Michigan tested every incarcerated person in its state prison system in fewer than 15 days.

